Depth of Anesthesia
Introduction
General anesthesia is a medically induced state of unresponsiveness and unconsciousness. This state facilitates the safe and effective conduct of surgical procedures. The ability to assess adequate sedation is of utmost importance to get patients through surgery safely. In 1937, Dr. Arthur Guedel described the stages of anesthesia, providing a framework of clinical signs and typical behaviors that allow the anesthesiologist to reliably determine their patients' depth of sedation. These stages were described using ether as the primary anesthetic. Although ether is no longer used, the classification is still pertinent to modern anesthesia practice.
Anesthesia stages (Guedel's classification)[1]
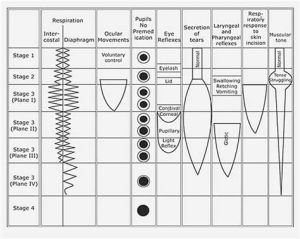
Stage 1: Analgesia or disorientation
This stage is marked by the preoperative anesthesia state to unconsciousness. During this stage, the patient may be sedated but still conversational and conscious. It can be described as the "induction stage" or the "disorientation stage", in which respirations are slow and regular, eye movement is voluntary, and muscular tone is normal.
Stage 2: Excitement or Uninhibited response
In this stage, the patient may present with tense struggling, vomiting, breath holding, coughing and swallowing. Airway reflexes remain intact during this phase, and can be hypersensitive to manipulation. Therefore, manipulation of airway (placement or removal of endotracheal tubes, suctioning) should be avoided, in order to prevent laryngospasm. This stage is characterized by loss of eyelash reflex and outward movement of the eye. This stage can be minimized with fast acting agents, psychological preparation of patient and quiet surroundings.
Stage 3: Surgical anesthesia
This stage starts with mechanical ventilation and respiratory paralysis. It is marked by decreased response to surgical incision. Guedel has divided this stage into four planes:
- Plane 1: from onset of automatic respiration to cessation of eye movement. Eyelid, conjunctival and swallow reflexes disappear.
- Plane 2: from cessation of eye movement to start of intercostal paralysis. Corneal and laryngeal reflexes disappear. Increased lacrimation may occur.
- Plane 3: from start of intercostal paralysis to complete paralysis. Pupillary light reflex disappears. This plane is referred as the "true surgical anesthesia", in which the response to incision is minimal.
- Plane 4: from complete intercostal paralysis to diaphragmatic paralysis. Apnea.
Stage 4: Overdosage
This stage is marked by apnea and loss of all reflexes, and may lead to death. Cardiovascular and respiratory support are necessary in this stage. Pupils are widely dilated due to increased levels of adrenaline. Maximum dilation is characterized by anoxia and paralysis of the sphincter.
Awareness during anesthesia
Awareness during general anesthesia occurs when depth of anesthesia is inadequate to achieve a state of unconsciousness.[2] It is characterized by recall of events during surgery, ranging from auditory to painful stimulation memories. The incidence ranges from 1:1,000 to 1:20,000,[3] being difficult to assess due to investigation dependent incidence. It is most common during induction and emergence of general anesthesia.
There are some risk factors that may contribute to this complication, and they are related to:
Anesthesia technique:
- use of neuromuscular blockade medications (decreased perception of awareness when patient is paralysed)
- total intravenous anesthesia (TIVA) - (human error, pump or IV defect)
Surgical procedure:
- emergency surgery (hemodinamic instability that reduces delivery of anesthetic, lower dosage of anesthetics)
- emergency cesarian section (lower dosage of anesthetics and inadequate delivery of anesthetic because of rapid incision)
- difficult airway placement (volatile agents may not be delivered until placement of definitive airway)
- cardiopulmonary bypass (altered physiology and volatile agents are stopped)
Patient:
- history of awareness
- genetic resistance to anesthetics
- chronic substance abuse (resistance to anesthetics)
- obese
- congestive heart failure or significant valvular disease (reduction of dosage of anesthetics)
Intraoperative monitoring
Clinical features:
Heart rate, blood pressure, purposeful movement and end tidal anesthetic concentration (ETAC) may be useful in recognizing awareness during general anesthesia. However, some drugs may mask these signs (calcium channel blockers, neuromuscular blockers).
Bispectral index (BIS):
Processed EEG monitor, translating EEG waves into a numeric scale ranging from 0 (complete EEG suppression) to 100 (fully awake). It is said that adequate anesthesia may be present with a BIS value of 40-60. Studies have shown that intraoperative BIS, compared to clinical signs, may have a reduction of intraoperative awareness (OR) 0.36, 95% CI 0.21 to 0.60; I2 = 61%; 27 studies; 9765 participants[4], time to eye opening, time to orientation, and time to discharge patient from PACU[4]. However, BIS guided anesthesia did not show a clinical difference to anesthesia guided by end tidal anesthetic gas concentration (ETAC). Furthermore, studies show that neuromuscular blockade alone, without other anesthetics, decrease the value of BIS.[5] Therefore, the accuracy and reliability of BIS are questionable.
SEDline®:
Processed EEG monitor. The PSI (Patient State Index) translates the effect of anesthetic drugs in humans into a numeric scale ranging from 0 (complete EEG suppression) to 100 (fully awake). The target value for general anesthesia is between 25-50. A study showed that this monitor better captured changes in brain state from dexmedetomidine sedation, compared to RASS score and SEF95[6]. Another study suggests that PSI may be adequate to monitor anesthesia with sevoflurane in the pediatric population, when compared to the BIS monitor<ref>Usefulness of bispectral index and patient state index during sevoflurane anesthesia in children: A prospective observational study
Relevant Article Depot:
Open Anesthesia: Stages of Anesthesia
Bispectral index for improving intraoperative awareness and early postoperative recovery in adults
Depth of anaesthesia monitoring: updated evidence. Comment
Depth of anaesthesia monitoring: time to reject the index? Depth of amnesia monitoring. Response to Br J Anaesth 2023; 131: e145–7
Consciousness and General Anesthesia: Challenges for Measuring the Depth of Anesthesia
Limitations of anaesthesia depth monitoring
Age-dependency of sevoflurane-induced electroencephalogram dynamics in children
A Window into the Developing Brain: Toward a Deeper Understanding of Pediatric Anesthesia
Depth of Anesthesia Monitoring
Consciousness and General Anesthesia: Challenges for Measuring the Depth of Anesthesia
Accidental awareness during anesthesia in children
References
- ↑ Atkison, R.S., Rushman, G. B., Lee, J. Alfred, A synopsis of anaesthesia
- ↑ Intraoperative and Anesthesia Awareness https://www.ncbi.nlm.nih.gov/books/NBK582138/#:~:text=Awareness%20under%20anesthesia%20is%20a,achieve%20a%20state%20of%20unconsciousness.
- ↑ Sebel PS, Bowdle TA, Ghoneim MM, Rampil IJ, Padilla RE, Gan TJ, Domino KB. The incidence of awareness during anesthesia: a multicenter United States study. Anesth Analg. 2004 Sep;99(3):833-839
- ↑ 4.0 4.1 https://pubmed.ncbi.nlm.nih.gov/31557307/
- ↑ Schuller PJ, Newell S, Strickland PA, Barry JJ. Response of bispectral index to neuromuscular block in awake volunteers. Br J Anaesth. 2015 Jul;115 Suppl 1:i95-i103.
- ↑ EEG response of dexmedetomidine during drug induced sleep endoscopy https://pubmed.ncbi.nlm.nih.gov/37521700/