One Lung Ventilation: Difference between revisions
No edit summary |
No edit summary |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 179: | Line 179: | ||
[https://link.springer.com/article/10.1007/s12630-024-02709-1 Manual angulation of the Arndt endobronchial blocker to improve the ease of lung isolation] | [https://link.springer.com/article/10.1007/s12630-024-02709-1 Manual angulation of the Arndt endobronchial blocker to improve the ease of lung isolation] | ||
[https://link.springer.com/article/10.1007/s12630-024-02767-5 A novel maneuver to correct the position of an EZ-Blocker® endobronchial blocker] | |||
[https://www.cureus.com/articles/293539-effects-of-dexmedetomidine-in-improving-oxygenation-and-reducing-pulmonary-shunt-in-high-risk-pediatric-patients-undergoing-one-lung-ventilation-for-thoracic-surgery-a-double-blind-randomized-controlled-trial Effects of Dexmedetomidine in Improving Oxygenation and Reducing Pulmonary Shunt in High-Risk Pediatric Patients Undergoing One-Lung Ventilation for Thoracic Surgery: A Double-Blind Randomized Controlled Trial] | |||
[https://journals.lww.com/anesthesia-analgesia/fulltext/2024/12000/point_of_care_lung_ultrasound_to_evaluate_lung.24.aspx Point-of-Care Lung Ultrasound to Evaluate Lung Isolation During One-Lung Ventilation in Children: A Blinded Observational Feasibility Study] | |||
Latest revision as of 23:55, 18 November 2024
Introduction
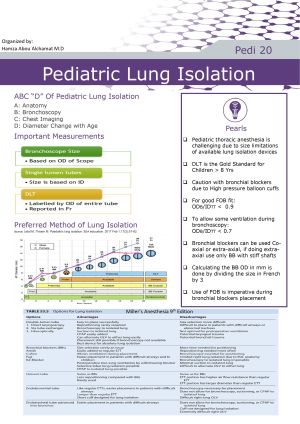
- Pediatric thoracic anesthesia is more challenging than Adults
- DLT is gold standard for children > 8 Yrs
- Available devices for Peds OLV: DLT, BB, Uninvent Tubes, SLT
- Caution with BB due to high pressure balloon cuffs - Many surgical procedures in the chest need OLV, but some can be done without it
ABC”D” OF Pediatric Lung isolation
| ABC"D" of Pediatric Lung Isolation | |
|---|---|
| A | Anatomy |
| B | Bronchoscopy |
| C | Chest imaging |
| D | Diameter change with age |
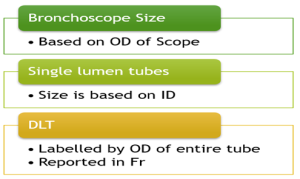
Important measurements
- How to know if FOB fits in the Tube?
ODB/IDTT < 0.9
- To allow some ventilation during bronchoscopy
ODB/IDTT < 0.7
Example: smallest FOB in use has OD of 2.2 mm, placing this Scope through 2.5 SLT gives an ODB/IDTT ratio of 2.2/2.5 or 0.88
This ratio is <0.9 but >0.7, the bronchoscope will physically fit inside the TT, but no ventilation will be able to occur!
Tip: Bronchoscopes can become deformed from repeated use and cleaning, and the tip may have a larger diameter than documented
>>> It’s always a good idea to test the fit of the bronchoscope inside a TT before use in the patient
Pediatric Airway Diameters
- Average neonatal trachea has an AP diameter of about 4.3 mm for both males & females
- Trachea grows uniformly in males and females to about 14 mm at the age of 15 yrs old
- At this time, female trachea stops growing, but male trachea continues to grow to 16–18 mm by age of 19
- trachea is elliptical in shape, with the transverse diameter being larger than AP diameter Sizing of airway devices should be based on the smaller (anteroposterior) diameter.
Devices & Approaches
1- Single-Lumen Tracheal Tube
- Simplest option, can be used at any age but mostly used for the very young patients < 6 m.o.s
- Placing SLT in the right mainstem bronchus is easier than the left due to the less acute angle that it takes off from the trachea
- Pros: Simple/ Quick
- Cons: potential for inadequate collapse of operative lung / inability to suction the operative lung / inability to deliver (CPAP) to operative lung / Missing the RUL when doing right mainstem intubation
2- Bronchial Blockers
- Many types, include vascular balloon catheters, the Uniblocker (Fuji Systems), and Arndt endobronchial blocker, Cohen, EZ blocker
- Catheters may be placed either within (Coaxial) or external to the TT (Extra-axial)
- Use of Bronchoscope is imperative during placement of BB
- Deflation of the operative lung occurs by absorption atelectasis and requires a considerably longer period of time
Vascular Devices:
- Fogarty arterial embolectomy catheter, and Miller atrio-septostomy catheter
- No central channel for deflation or CPAP to the operative lung
- Both has angled tip which allows the user to direct the catheter to the desired bronchus.
- Balloon cuffs are high pressure, low volume and should be only inflated and positioned under FOB to avoid damaging bronchial mucosa
Arndt blockers:
- Has four-way adapter, and comes with swivel connector that allows ventilation during placement
- The blocker has a 2 ml cuff and lower inflation pressures.
- Has an inner lumen that contains a flexible nylon wire that extends along the length of the catheter and terminates as a flexible loop
- This loop slides over the bronchoscope and aids in positioning.
- Once the nylon guide is removed, it cannot be reattached, which may make repositioning attempts difficult should the blocker fall out of place.
- Once the nylon wire is removed, the central lumen may be used for suctioning and CPAP
Sizing of BB and FOB for SLTs
- Same sizing principles apply when using BB and FOB together as to when sizing FOB alone
- Typically in pediatrics, two sizes of bronchial blockers are used—5 and 7 Fr BB sized by Fr, divide by 3 to know the size in mm
- When using the coaxial technique, the Arndt bronchial blocker works well.
- However, when using the parallel technique, a bronchial blocker with a stiffer shaft and angled tip should be used.
- This can be accomplished with the 5 Fr Fuji Uniblocker, or a vascular device such as a 5 Fr Fogarty embolectomy catheter, or a 5 Fr Miller atrio-septostomy catheter
3- Univent Tubes
- TT that has a bronchial blocker within a separate lumen.
- If double-lung ventilation is required again, the bronchial blocker may be deflated and withdrawn into the tracheal lumen again
- Available Univent pediatric sizes: 3.5 and 4.5 mm ID
- Size of a Univent TT refers to the ID, where the OD will be much larger than the equivalent sized SLT
- Main disadvantage is that cross-sectional diameter of the ventilation lumen is smaller in order to accommodate the blocker lumen.
- This increases airway resistance and also limits the size of fiberoptic bronchoscope used to facilitate positioning
- Narrow age range where this method is the preferred: 6–8 yrs
4- Double Lumen Tubes
Considered Gold standard in ages > 8 yrs
The equation of Size =Age×1.5+14 can help to estimate the sizing needed
Smallest DLT size is a 26 Fr, which is generally suitable for children 8–10 yrs of age
Recommended method for each age group
A table listing the preferred method for lung isolation in each age group can be found in the Info sheet at the bottom of this page
This is a Stub Notice. This page has not been completed. You can work on this page by signing in and going to the Edit tab. Thanks for helping to make PedsAnesthesia.Net Wiki useful.
Go to the Main Page to see the Topic Outline.
Go to the Generalized Suggested Outline for information on case-specific details for each page.
Go to the Test Page for examples on how to use references in the page.
Relevant Article Depot:
Single-lung ventilation in infants and children
Hypoxemia in Young Children Undergoing One-lung Ventilation: A Retrospective Cohort Study
Anesthesia of thoracic surgery in children
Single lung ventilation with an endotracheal tube in a small child undergoing right thoracotomy
Error traps in pediatric one-lung ventilation
Radiographic Demonstration of Hypoxic Pulmonary Vasoconstriction during One-lung Ventilation
Cricoid and left bronchial diameter in the pediatric population
Hypoxaemia during one lung ventilation
Double-lumen tubes and bronchial blockers
Manual angulation of the Arndt endobronchial blocker to improve the ease of lung isolation
A novel maneuver to correct the position of an EZ-Blocker® endobronchial blocker