Intraoperative Cardiac Arrest: Difference between revisions
No edit summary |
No edit summary |
||
| Line 82: | Line 82: | ||
* Avoid hypoglycemia | * Avoid hypoglycemia | ||
* Avoid hyperventilation (unless herniating) | * Avoid hyperventilation (unless herniating) | ||
'''<u>Special Considerations:</u>''' | |||
'''LARYNGOSPASM:''' | |||
* On induction, 100% FiO2, deepen anesthetics | |||
* IM atropine 0.02 mg/kg (0.1 mg minimum dose) and | |||
* IM succinylcholine 4 mg/kg (maximum dose 150 mg). | |||
* If the patient has IV or IO access, then a lower dose of succinylcholine should be used to break laryngospasm (0.3–1.0 mg/kg) | |||
* Of note, don’t need to aspirate before IM injection | |||
'''VP SHUNT:''' | |||
During chest compressions: | |||
* Without increased ICP: one-third of the intrathoracic pressure generated may be transmitted to the ICP via the vertebral veins and CSF | |||
* With increased ICP much higher percentage of intrathoracic pressure during chest compressions is transmitted to ICP, significantly decreasing cerebral perfusion pressure. | |||
Neurosurgeon should immediately tap the VP shunt to remove cerebrospinal fluid (CSF) and reduce ICP. | |||
'''VENOUS AIR EMBOLUS:''' | |||
Administering 100% inspired oxygen | |||
Discontinuing nitrous oxide and inhaled drugs | |||
Stopping air entry: | |||
* Flood field with fluid | |||
* Lower field to promote venous filling | |||
* Trap air in right atria (right side up) | |||
Aspirating air from the central line | |||
CPR and vasopressor administration may be needed | |||
'''HYPERKALEMIA''' | |||
The acute resuscitation to drive potassium into cells and reduce cardiotoxicity includes (Mnemonic: C-B-I-G) | |||
Calcium CaCl2 20 mg/kg or Calcium Gluconate 60 mg/kg IV or IO | |||
Bicarb: NaHCO3 1–2 mEq/kg IV or IO | |||
Insulin/Glucose: D25 W 2 mL/kg and regular insulin 0.1 U/kg | |||
Alkalosis Hyperventilation (can see immediate decrease in T waves) | |||
'''LOCAL ANESTHETICS TOXICITY''' | |||
Seizure: immediate treatment with benzodiazepine | |||
Cardiac arrest: chest compressions should be started and Epi at low initial doses (1 μg/kg based on adult recommendations). | |||
Antiarrhythmic drugs: amiodarone (avoid lidocaine and procainamide) | |||
Intralipid: | |||
1.5 mL/kg bolus of 20% intralipid over 1 minute | |||
If HDS, infusion at 0.25 mL/kg/min for 10 minutes | |||
If still unstable: additional 1.5 mL/kg bolus, then infusion rate at 0.5 mL/ kg/min | |||
Max total dose 10 mL/kg of lipid emulsion over 30 minutes | |||
'''ANAPHYLAXIS:''' | |||
Remove the likely allergens | |||
Administering 100% oxygen | |||
Epinephrine: | |||
10 μg/kg/dose IM up to 0.5 mg/dose q 20 minutes or IV infusion | |||
IVF (boluses of 20 mL/kg) | |||
Trendelenburg positioning | |||
Histamine blockers, Albuterol and corticosteroids | |||
Serum tryptase level is a useful indicator that mast cell degranulation occurred. The test for serum tryptase is time sensitive and needs to be obtained within 3 hours | |||
'''<u>Critical Event Resources:</u>''' | '''<u>Critical Event Resources:</u>''' | ||
Revision as of 17:46, 18 November 2023
Incidence of Perioperative Cardiac Arrest (CA):
Increase with higher ASA status
Wake Up Safe Registry: 3.3 per 10,000 of arrest were anesthesia related. Aesthesia-related death was 0.36 per 10,000 anesthetics.
Pediatric Perioperative Cardiac Arrest (POCA) Registry: 1.4 +/- 0.45 per 10,000 were anesthesia related. Mortality rate: 26%
Children (<12 year old): 2x more likely to experience CA, infants (<1 year old): 10x, neonates (<1month old): 50x
Causes for Pediatric Perioperative Arrest:
- CIRCULATORY FAILURE:
- Hypovolemia: Hemorrhage, inadequate/inappropriate volume resuscitation/transfusion (patients < 24 months may not respond to hypotension with increase HR)
- Hyperkalemia: Succinylcholine, TRANSFUSION (pRBC >2 weeks, speed of transfusion), reperfusion, myopathy, or renal insufficiency
- Dysrhythmia: LA toxicity, line placement (safer to use Ultrasound guided vs. landmark technique)
- Anaphylaxis
- Venous Air Embolism
- Malignant Hyperthermia: very rare
- RESPIRATORY FAILURE:
- Airway Obstruction: - Laryngospasm: Upper respiratory infection increases risk - Bronchospasm
- Inadequate ventilation and oxygenation: difficult airway, mucus plug, kinked ETT, inadvertent extubation
- Disordered control of breathing: drug overdose, neuromuscular diseases, apnea
- Aspiration
- SUDDEN CARDIAC COLLAPSE
- Bradycardia or cardiovascular collapse: - Traction, pressure, or insufflation involving the abdomen, eye, neck, or heart - Undiagnosed cardiomyopathy
- Overdose - Weight-based dosing of IV anesthetic on induction in a child with hypovolemia or compensated shock may lead to collapse
Important Resuscitation Steps:
- Inform team
- Stop surgical stimulation
- Stop anesthetics (gas & sedation gtt) and vasodilatory meds
- 100% Oxygen
- Open fluids and Trendelenburg position
- Chest-compression
- Call for help
- Consider stopping potassium containing solutions (blood or hyperalimentation)
- Ask for ice to head
- Assign roles
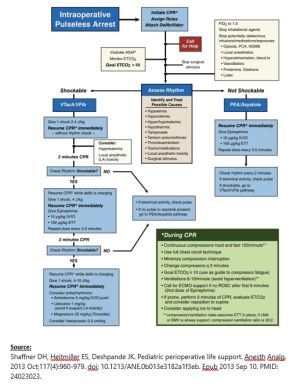
Resuscitation Algorithm for Intraoperative Pulseless Arrest:
Source: Shaffner DH, Heitmiller ES, Deshpande JK. Pediatric perioperative life support. Anesth Analg. 2013 Oct;117(4):960-979. doi: 10.1213/ANE.0b013e3182a1f3eb. Epub 2013 Sep 10. PMID: 24023023.
Important Notes:
- Medication have not been shown to change outcome, more emphasis on effective compression.
- Compression depth:
- For a child is at least ⅓ the depth of the chest size, or 5 cm
- For infant: 4cm
- Allow complete recoil, don’t lean on chest
- Don’t interrupt compression
- Intubate, follow ETCO2
- 100 compressions : 8-10 ventilations per min
- Avoid overinflation
- Biphasic shock - First dose: 2-4J/kg - Second dose: 4J/kg - Third dose: 4-10J/kg
- Epi dose: - 10 MICROg/kg IV/IO - 100 MICROg/kg ETT
- PEA vs. VFib rhythm: PEA appears organized and pulseless
- Call for ECMO if no ROSC after 6 mins
- Ice to head
- If prone, perform 2 mins CPR prone, evaluate EtCO2 then consider supine
- IO access is as effective as IV access and may be easier to obtain during circulatory collapse
Methods of Measuring Effectiveness of CPR
- ETCO2 levels >10 mm Hg are associated with higher likelihood of ROSC
- >30mmHg: good
- <10 mmHg: bad
- Diastolic pressure on a-line (relaxation right atrial pressure):
- >20 mmHg infants
- >30 mmHg children
- <15 mmHg - bad (in adults associated with no ROSC during CPR)
- MVO2
- <30% was associated with no ROSC
Post Resuscitation:
- Avoid hypotension
- Allow to be cool (avoid hyperthermia)
- Avoid hypoglycemia
- Avoid hyperventilation (unless herniating)
Special Considerations:
LARYNGOSPASM:
- On induction, 100% FiO2, deepen anesthetics
- IM atropine 0.02 mg/kg (0.1 mg minimum dose) and
- IM succinylcholine 4 mg/kg (maximum dose 150 mg).
- If the patient has IV or IO access, then a lower dose of succinylcholine should be used to break laryngospasm (0.3–1.0 mg/kg)
- Of note, don’t need to aspirate before IM injection
VP SHUNT:
During chest compressions:
- Without increased ICP: one-third of the intrathoracic pressure generated may be transmitted to the ICP via the vertebral veins and CSF
- With increased ICP much higher percentage of intrathoracic pressure during chest compressions is transmitted to ICP, significantly decreasing cerebral perfusion pressure.
Neurosurgeon should immediately tap the VP shunt to remove cerebrospinal fluid (CSF) and reduce ICP.
VENOUS AIR EMBOLUS:
Administering 100% inspired oxygen
Discontinuing nitrous oxide and inhaled drugs
Stopping air entry:
- Flood field with fluid
- Lower field to promote venous filling
- Trap air in right atria (right side up)
Aspirating air from the central line
CPR and vasopressor administration may be needed
HYPERKALEMIA
The acute resuscitation to drive potassium into cells and reduce cardiotoxicity includes (Mnemonic: C-B-I-G)
Calcium CaCl2 20 mg/kg or Calcium Gluconate 60 mg/kg IV or IO
Bicarb: NaHCO3 1–2 mEq/kg IV or IO
Insulin/Glucose: D25 W 2 mL/kg and regular insulin 0.1 U/kg
Alkalosis Hyperventilation (can see immediate decrease in T waves)
LOCAL ANESTHETICS TOXICITY
Seizure: immediate treatment with benzodiazepine
Cardiac arrest: chest compressions should be started and Epi at low initial doses (1 μg/kg based on adult recommendations).
Antiarrhythmic drugs: amiodarone (avoid lidocaine and procainamide)
Intralipid:
1.5 mL/kg bolus of 20% intralipid over 1 minute
If HDS, infusion at 0.25 mL/kg/min for 10 minutes
If still unstable: additional 1.5 mL/kg bolus, then infusion rate at 0.5 mL/ kg/min
Max total dose 10 mL/kg of lipid emulsion over 30 minutes
ANAPHYLAXIS:
Remove the likely allergens
Administering 100% oxygen
Epinephrine:
10 μg/kg/dose IM up to 0.5 mg/dose q 20 minutes or IV infusion
IVF (boluses of 20 mL/kg)
Trendelenburg positioning
Histamine blockers, Albuterol and corticosteroids
Serum tryptase level is a useful indicator that mast cell degranulation occurred. The test for serum tryptase is time sensitive and needs to be obtained within 3 hours
Critical Event Resources:
PEDI CRISIS APP
Available on Apple Store and Google Play
https://pedsanesthesia.org/pedi-crisis-app/
This is a Stub Notice. This page has not been completed. You can work on this page by signing in and going to the Edit tab. Thanks for helping to make PedsAnesthesia.Net Wiki useful.
Go to the Main Page to see the Topic Outline.
Go to the Generalized Suggested Outline for information on case-specific details for each page.
Go to the Test Page for examples on how to use references in the page.
Relevant Article Depot:
This is a Stub Notice. This page has not been completed. You can work on this page by signing in and going to the Edit tab. Thanks for helping to make PedsAnesthesia.Net Wiki useful.
Go to the Main Page to see the Topic Outline.
Go to the Generalized Suggested Outline for information on case-specific details for each page.
Go to the Test Page for examples on how to use references in the page.
Relevant Article Depot: